IU Medical Researchers Present Promising Cancer Study Results
Photography Provided
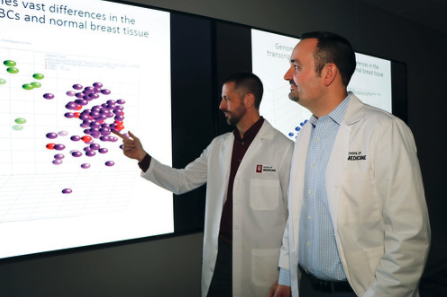 Anyone who has beaten breast cancer, or any cancer for that matter, likely often wonders, “What if it comes back?” Two Indiana University School of Medicine researchers, Dr. Bryan Schneider and Dr. Milan Radovich, have exciting new findings, however, that spell good news for cancer patients.
Anyone who has beaten breast cancer, or any cancer for that matter, likely often wonders, “What if it comes back?” Two Indiana University School of Medicine researchers, Dr. Bryan Schneider and Dr. Milan Radovich, have exciting new findings, however, that spell good news for cancer patients.
Schneider and Radovich Two Indiana University School of Medicine researchers came up with a biomarker finding for women diagnosed with triple-negative breast cancer that is now being taught and used worldwide.
This pioneering research is part of the larger IU Precision Health Initiative, which received $120 million in funding from the IU Grand Challenges Program to research diseases such as Alzheimer’s, Type 2 diabetes, multiple myeloma and pediatric sarcomas (childhood cancers).
According to Schneider, breast cancer remains one of the most common cancer types for women in the U.S., with more than 250,000 women affected annually and approximately 40,000 dying of the disease. Triple-negative breast cancer tends to target young women and black women. Because it’s an aggressive form of breast cancer, even though it makes up a minority of cases, it causes a disproportionately high rate of mortality.
“Women with triple-negative breast cancer who had Stage 1 through 3 disease are treated with chemo followed by surgery,” says Radovich, noting that there are two post-surgical outcomes. Either chemotherapy melts all of the tumor away (this occurs in approximately one-third of patients), or patients have residual disease post-surgery.
 “Even though we remove that cancer, they are at high risk of their cancer coming back, usually with a vengeance as the disease has metastasized to other organs and becomes lethal,” Radovich says.
“Even though we remove that cancer, they are at high risk of their cancer coming back, usually with a vengeance as the disease has metastasized to other organs and becomes lethal,” Radovich says.
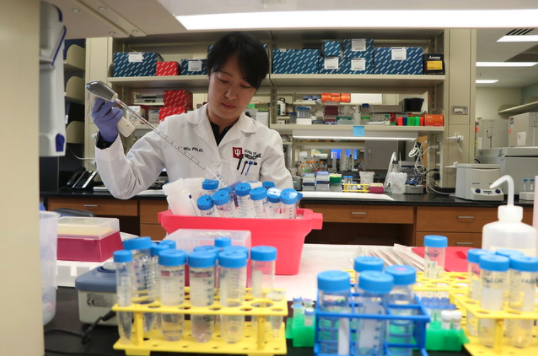
Schneider and Radovich analyzed ctDNA (circulating tumor DNA), which is DNA shed from tumors into the bloodstream. With cutting-edge technology from https://www.rondaxe.com/, a blood sample could be taken and the presence of cancer detected.
“We found that if we take this blood sample after surgery and radiation, and we detect this tumor DNA, those women’s cancer will recur,” Schneider says. “If they are negative, those women have a good chance that the cancer won’t come back and therefore have a better, superior outcome.”
Physicians in the cancer-fighting world are eager to hear more about these findings, as the concept of using a blood-based biomarker to predict where cancer will come back is being used across other cancers as well. In December of 2019, Radovich presented this data in front of a packed audience of 12,000 at the San Antonio Breast Cancer Symposium. In addition, the work of Schneider and Radovich was published in JAMA Oncology, a peer-reviewed medical journal published by the American Medical Association.
“The real goal behind this is to take care of those patients who are in a tough situation,” Radovich says. “For those patients who are ctDNA-negative, you can tell them that they are in a situation where there is a really good chance of doing well, which provides a sense of relaxation and comfort. It also allows us the potential to think about strategies down the road that deescalate the amount of therapy patients get, so they suffer fewer side effects.”
For those deemed high-risk, physicians can implement innovative strategies in an attempt to improve outcomes.
“As Hoosiers, we should be proud of what our state is doing in advancing research that has implications across the country and internationally,” Radovich says. “IU has been a leader in this concept of using DNA and genomics to guide therapy for more than 20 years, long before it had become a hot topic in the New York Times or Time magazine. What you’re seeing today is an evolution of decades of work in this area.”
In addition to ctDNA, doctors also looked at circulating tumor cells in the study. Much of that work came out of Purdue University.
“It’s a really neat collaboration both here in the state and across the United States,” says Schneider, who is starting a new clinical trial with Radovich called the Persevere Trial.
Based on the newly established ctDNA findings, the new national trial will involve 200 women with triple-negative breast cancer in 20 sites across the U.S.
 According to Schneider, the sequencing of the first human genome propelled much of science to where it is today.
According to Schneider, the sequencing of the first human genome propelled much of science to where it is today.
“When the first human’s entire blueprint was mapped out, that set the stage for the entire code for which we’re built and how cancer is formed,” Schneider says. “As we have the ability to use genomes in real time in a few days for much cheaper, we’re starting to learn in a logarithmic fashion. Now we are starting to see the fruits of that labor.”
Radovich adds that scientists can now sequence a genome in a couple of days for a few hundred dollars.
“It’s unbelievable how commoditized and quick it has become, and how applicable it is to patient care,” Radovich says. “Dr. Schneider and I are proud to lead our genomics program. We apply genomics to patients with cancer here at IU Health.”
To date, they have sequenced more than 5,000 patients.
“It’s been a game-changer to tailor therapy for individual patients,” Radovich says. “We imagine a day where genome sequence can be done at your bedside or as part of your routine visit with your doctor. Your genome analysis can then help guide therapies.”
Both doctors say they feel blessed to have the opportunity to deal with patients during a difficult journey.
“We get to see the limitations in where we are, go back to the laboratory, and think about some of the things we can do and advances we make that we know will impact the patients when we see them next week,” Radovich says. “That’s an unbelievable feeling, and one that we are incredibly passionate about.”